The West Nile Virus (WNV) first appeared in the United States in 1999, when tests confirmed that a number of wild birds in the New York City area had been carriers of the virus. Since then, WNV has spread across the continental United States, with only 2 states not reporting WNV activity in 2003.
WHAT SPECIES ARE AFFECTED BY WNV?

Humans, equidae and wild birds are most commonly affected by WNV. There have been a few confirmed cases in livestock in the United States.
Pets: Clinical signs associated with West Nile virus infection in dogs, cats, domestic rabbits, and domestic birds have not been well described. It appears that these animals may be infected, but rarely develop clinical signs of disease. There were less than 40 dogs and 1 one cat reported infected with WNV to CDC during 2003. Experimentally infected dogs showed no symptoms after infection with WNV, while some experimentally infected cats exhibited mild, non-specific symptoms during the first week after infection, such as low grade fever and lethargy.
There is no documented evidence of person-to-person or animal-to-person transmission of WNV. Because WNV is transmitted by infectious mosquitoes, dogs or cats could be exposed to the virus in the same way humans become infected. Veterinarians should take normal infection control precautions when caring for an animal suspected to have this or any viral infection. It is possible that dogs and cats could become infected by eating dead infected animals such as birds or mice. Studies have shown that cats have become infected with the virus after eating infected mice, but they generally do not show any sign of illness.
Do NOT use DEET-based repellents on pets. Animals tend to lick themselves and ingest the product, potentially causing health problems. Use species-appropriate repellent products. Ask your veterinarian which products are most likely to be both safe and effective.
There is currently no vaccine approved for use in dogs and cats, and there is no specific treatment for WNV infection. Treatment is supportive and consistent with standard veterinary practice for animals with a viral infection. There is no reason to destroy an animal just because it is infected with WNV. Full recovery from the infection is likely. Please visit with your veterinarian for additional information.
Horses: Cases of WN virus disease in horses have been documented, either by virus isolation or by detection of WN virus-neutralizing antibodies in 1999, 2000, 2001, 2002, and 2003. Approximately 40% of equine WN virus cases results in the death of the horse. The horses most likely became infected with WN virus in the same way humans become infected, by the bite of infectious mosquitoes.
In locations where WN virus is circulating, horse should be protected from mosquito bites as much as possible. Horses vaccinated against eastern equine encephalitis (EEE), western equine encephalitis (WEE), and Venezuelan equine encephalitis (VEE) are NOT protected against WN virus infection. A West Nile virus vaccine for horses was recently licensed, but its effectiveness is unknown. Horses infected by WN virus develop a brief low-level viremia that is rarely, if ever, infectious to mosquitoes. There is no reason to destroy a horse just because it has been infected with WN virus. Data suggest that most horses recover from the infection. Treatment would be supportive and consistent with standard veterinary practices for animals infected with a viral agent.
Other Species: WNV has been reported to the CDC in many species of birds as well as several species of mammals and even reptiles. A short list of other mammals infected with WNV includes bats, chipmunks, bears, deer, lamas, alpacas, and domestic sheep as well as other species.
HOW IS THE DISEASE SPREAD?
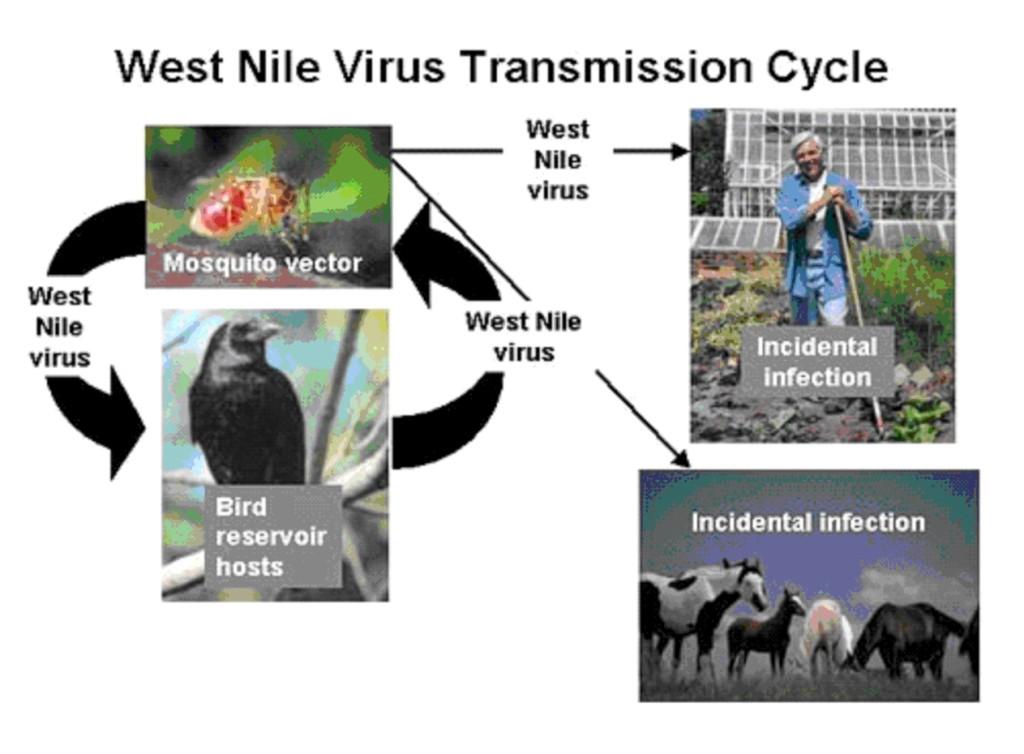
Wild birds represent the reservoir for this virus, which is transmitted by mosquitoes. After a mosquito bites an infected bird, the virus is retained in the mosquito's salivary glands. When the insect bites or feeds on a human or a horse, the virus is injected into the blood system where it multiplies and may cause the illness. Horses and humans are incidental hosts of WNV and therefore cannot transmit the disease.
WHAT ARE THE SYMPTOMS OF WNV?
Horses and other equidae will exhibit listlessness, stumbling and incoordination, weakness of limbs, ataxia, partial paralysis or death. A fever is not usually observed. Treatment would be supportive and consistent with standard treatment for animals infected with a viral agent. In humans, the most common symptoms are a fever and headache, but can include a rash, swollen nodes and conjunctivitis. In severe cases, the symptoms include the rapid onset of severe headache, high fever, stiff neck, disorientation, muscle weakness, coma or death.
IS THE DISEASE FATAL?
During the outbreak in 2000, 36 percent of the affected horses died or were euthanized. It is likely that horses recover from the infection without ever showing clinical signs of illness. Since horses are incidental hosts, affected animals do not need to be quarantined or euthanized. In 2001, there were 738 confirmed clinical cases in horses with at least 156 horses that died or were euthanized. The disease can also be fatal in humans.
HOW CAN I PROTECT ANIMALS AND MYSELF?
Preventing exposure to mosquitoes is essential. One of the best ways to do this is by removing any potential sources of water in which mosquitoes can breed.
This includes:
- Disposing of water-holding containers, including discarded tires
- Drilling holes in the bottom of containers that are left outside
- Cleaning clogged roof gutters
- Turning over plastic wading pools or wheelbarrows when not in use and do not allow water in bird baths to become stagnate
- Aerating ornamental pools or stocking them with fish
- Cleaning and chlorinating swimming pools that are not in use and being aware that mosquitoes can breed in the water that collects on swimming pool covers
- Landscaping property to eliminate standing water as mosquitoes can breed in any puddle that lasts more than four days
- Cleaning of livestock-watering troughs thoroughly on a monthly basis
PREVENTION FOR HORSES INCLUDES:
- Insect-proofing stables Insect-proofing stables Using insect repellant containing DEET
- Keeping animals inside during peak mosquito feeding hours (sunset to sunrise)
- Avoiding mosquito prone areas such as swampy areas and heavily forested areas
- Vaccinating animals
- Using fans may reduce the potential ability of mosquitoes to feed on horses
PREVENTION FOR HUMANS INCLUDES:
- Using insect repellant containing DEET
- Wearing long sleeves and pants when out-of-doors
- Avoiding mosquito prone areas such as swampy areas and heavily forested areas, especially between sunset and sunrise
IS THERE A VACCINE AVAILABLE?
There are 2 vaccines available for horses. The Fort Dodge West Nile-Innovator® is a killed vaccine that was given a conditional license in August 2001 and granted full licensure in February 2003. Merial released Recombitek® in January 2004 which is a recombinant canarypox vectored vaccine.
The Fort Dodge vaccine, West Nile-Innovator® is also available in four different combinations. Two formulations include tetanus along with various combinations of Easter equine encephalomyelitis (EEE), Western equine encephalomyelitis (WEE), and Venezuelan equine Encephalomyelitis (VEE). A recommendation of 2 initial doses of the vaccine give 3-6 weeks apart, given intramuscular will give protection at least 6 weeks after the second dose. An annual booster is needed.
Recombitek®, the Merial product, is recommended to be given as two doses 4-6 weeks apart initially and a single yearly booster given. Protection has been reported as early as 2 weeks following the second initial dose. Recombitek® will produce an effective booster response in horses previously vaccinated with the West Nile-Innovator® if the vaccination was done as recommended by Fort Dodge. This vaccine has not been tested in pregnant mares.
Horse owners should consult with their veterinarian concerning WNV vaccination of their horses.
WHAT ARE THE HUMAN HEALTH IMPLICATIONS?
Fact sheets about West Nile virus and human health can be accessed at the ND Department of Health & Human Services website or the Centers for Disease Control and Prevention website at www.cdc.gov.
Related Resources
West Nile Virus Contacts
North Dakota State Board of Animal Health
State Board of Animal Health
600 E Boulevard Ave.
Dept.602
Bismarck, ND 58505-0020
701-328-2655
Fax: 701-328-4567

